
A mother who was diagnosed with a rare and life-threatening blood disorder and needed to have her entire body’s worth of plasma replaced just four days after surviving an emergency C-section has thanked plasma donors for giving her a “second chance at life” as she looks to celebrate her son’s first birthday this summer.
Sophie Meredith, 33, from Shropshire, developed thrombotic thrombocytopenic purpura (TTP) during her pregnancy last year but was not officially diagnosed until after giving birth.
TTP is a rare blood disorder that causes overactive blood clotting and around six in 1,000,000 people are affected with the condition in the UK each year, the NHS says.
Sophie, a mental health therapist, had developed blood clots through her small blood vessels, which led to her platelets – cell fragments in the blood – dropping “dangerously low”.

During labour on July 17, her veins had started to “shut down” and this led to her needing an emergency C-section at Telford Hospital on July 18.
Sophie said she “felt like (she) was dying” as her “body was going into complete shutdown mode”, and doctors informed her that she and her son Arlo might not make it.
Although they survived, Sophie’s health deteriorated and she was blue-lighted to Queen Elizabeth Hospital on July 22, where she was diagnosed with TTP and had four plasma exchanges.
Within three days, Sophie’s entire body’s worth of plasma was removed and replaced with healthy donor plasma, saving her life – and since making a full recovery, her main priorities are now being the best mother she can possibly be to Arlo and living in the moment, as she has realised “how fragile life is for all of us”.
“I remember when I was diagnosed on the ward, they said, ‘Oh, you’re literally one in a million’,” Sophie said.
“But without plasma, I wouldn’t be alive, it’s literally that simple.
“I genuinely have a moment every day when my brain goes quiet and I just think, ‘thank God for those strangers who decided, for whatever reason, to donate’.
“Without them, I wouldn’t have a second chance at life, and I’m just so grateful for them.”

Sophie explained she had a “healthy, normal pregnancy” up until one month before she was due to give birth in July 2023.
She had been experiencing unusual symptoms, including visual disturbances, confusion and short-term memory loss, but her concerns were initially dismissed as being pregnancy-related.
Just two weeks before going into labour, however, Sophie’s condition worsened.

“I didn’t know what day it was, I didn’t know what I’d done that day, I didn’t know where I’d been that day, where I was meant to be going,” Sophie explained.
“So, I text my partner and just said, ‘Look, I’m confused, what’s happened? Where have we been today? What am I meant to be doing?’ And he said, ‘What do you mean?’
“He said it was like speaking to somebody that had dementia.”
Sophie attended check-ups at Telford Hospital but it was not until she went into labour on July 17 that health professionals discovered the severity of her condition.

She underwent further blood tests and the results showed Sophie’s platelets were “dangerously low”.
From there, Sophie said it was “absolute carnage” as her veins had started to “shut down”, leading to an emergency C-section on July 18.
Prior to this, she had to sign a waiver as doctors explained that they did not know whether Sophie and Arlo, now six months old, would make it.
“I just remember saying to them, ‘Just do whatever you need to do to get my baby here safely, and please try your best and not to lose us both’,” Sophie said.
Sophie regained consciousness and was informed Arlo was well and healthy, but she was not able to have “the special moment” of holding her baby until 24 hours later.

She was “completely relieved” that they had both survived, but Sophie’s platelets were continuing to drop and doctors did not know why.
She had platelet transfusions, which only provided a temporary improvement, along with blood transfusions, but she then noticed a rash on her chest and lower back.
Sophie then started developing jaundice – and with doctors and nurses still perplexed, they sent her bloods to other hospitals, which led to the suggestion she might have TTP.
She continued: “I didn’t even know TTP existed, and I asked them, ‘What does that mean? Does that mean that I’m dying? Am I going to die?’
“They just gave me this look of, ‘We’re not really sure whether you’re going to pull through this or not’.”
On July 22, Sophie was blue-lighted to Queen Elizabeth Hospital in Birmingham, where she received an official diagnosis of TTP and was told she needed plasma exchanges.
TTP can have various causes – but in Sophie’s case doctors believe it was triggered by an autoimmune response to her pregnancy.
A nurse then explained that Sophie needed the plasma exchanges straight away, otherwise she would die.

“Being faced with your own mortality, not once but twice, it’s a really strange sensation,” Sophie said.
“The overwhelming feeling is fear and wanting to tell everybody you love exactly how much you love them, and how much you care for them.
“But my driving force was my baby. The entire time I was in hospital, I just thought, ‘I need to be back with my baby’.”
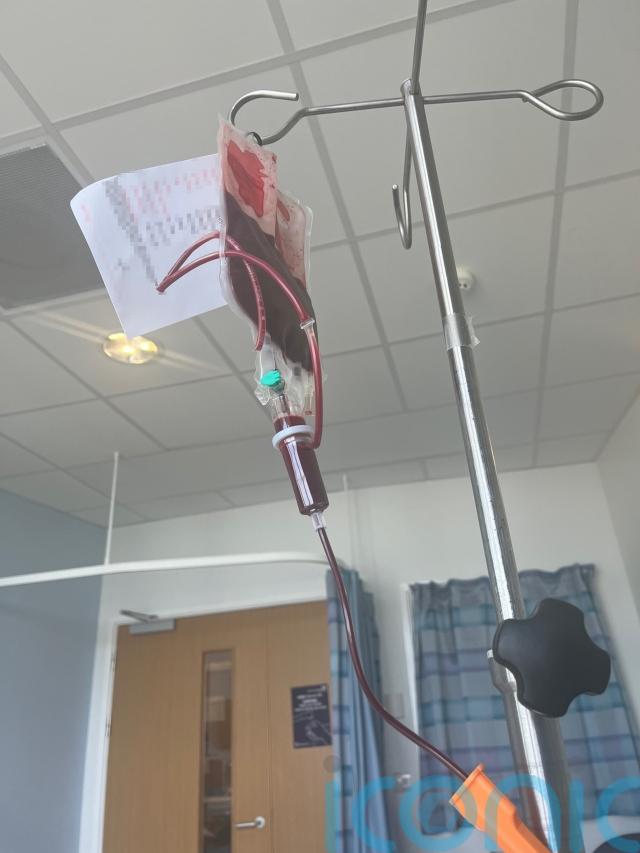
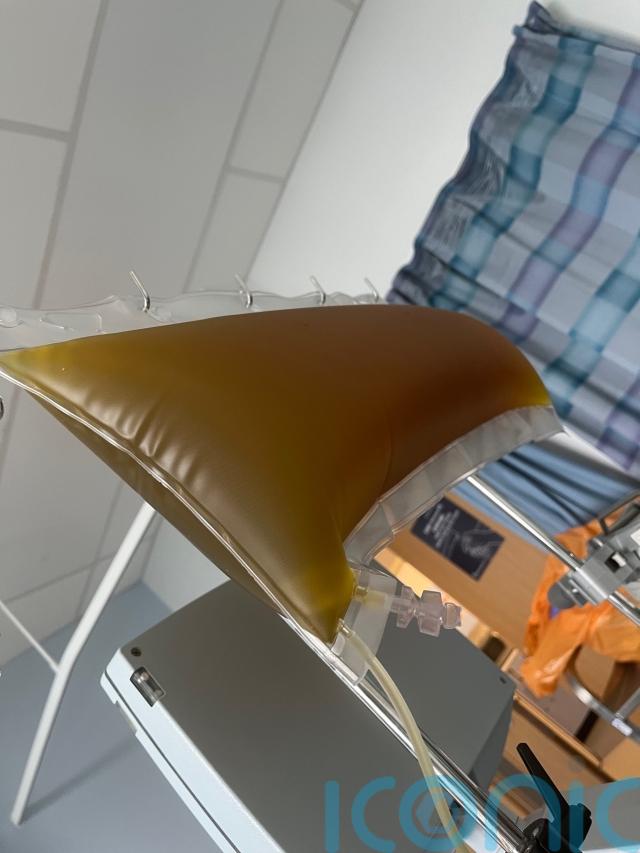
In total, Sophie received more than 27 bags of fresh frozen donor plasma via a catheter in her leg during four six-hour exchanges.

She also had the drug rituximab to treat the TTP and by day three her platelets had increased to a normal level.
On the fifth day, Sophie was discharged from hospital – and after continuing treatment at home for four weeks, she has since made a full recovery with no side effects.
Sophie now has to have blood tests every three months for the rest of her life, but she is classed as being in remission and feels extremely “lucky” to be alive.
She praised the “amazing” staff at Queen Elizabeth Hospital and the TTPNetwork, a UK patient-led organisation, for supporting her, but most importantly she wants to thank the plasma donors.
She described them as “superheroes” and since leaving hospital Sophie’s partner Dylan, 31, a facilities manager, has donated plasma as a way to “give back”.

Long-term, Sophie would like to set up a non-profit organisation that raises awareness of rare conditions, particularly those that can develop during pregnancy, to help others.
For now, however, she wants to urge people to “trust their gut and advocate for themselves” when it comes to their health, and she hopes her story will raise more awareness of TTP and the importance of plasma donations because, without them, she said she “wouldn’t be here” today.
“For people like me, (the plasma donors) have given me a second chance at life, they’ve given me the opportunity to raise my son,” Sophie said.
“I think people underestimate that they are genuinely saving lives … I’m a walking, talking example of that.”
For more information about blood and plasma donations, visit NHS Blood and Transplant’s website at: blood.co.uk/plasma
For more information about TTPNetwork, visit: ttpnetwork.org.uk
Subscribe or register today to discover more from DonegalLive.ie
Buy the e-paper of the Donegal Democrat, Donegal People's Press, Donegal Post and Inish Times here for instant access to Donegal's premier news titles.
Keep up with the latest news from Donegal with our daily newsletter featuring the most important stories of the day delivered to your inbox every evening at 5pm.