
A Northamptonshire man who was diagnosed with Parkinson’s in 2020 has “got his life back” thanks to a prescription for medical cannabis and hopes further research could help fellow Parkinson’s sufferers access the medication.
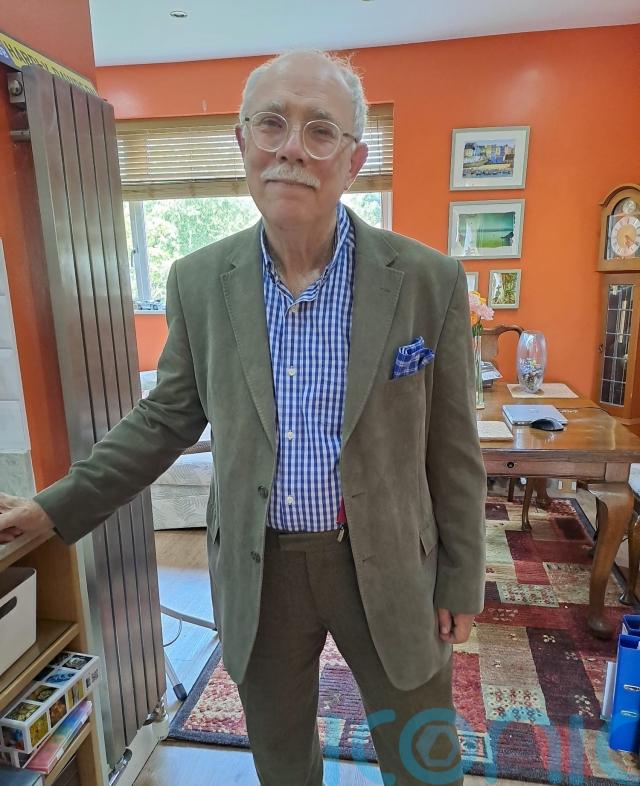
Steve Willis, 72, first noticed the signs of Parkinson’s – including tremors, difficulty swallowing, and micrographia, where his handwriting became much smaller – in June 2020. After being formally diagnosed by NHS doctors, he was prescribed Levodopa, a drug that is converted into dopamine in the brain to help with movement, which had limited effects on his quality of life.
A chance encounter with cannabis while on holiday in Jamaica in March 2025 – where the drug is decriminalised for personal use – led him to explore the possibility of accessing medical cannabis at home in the UK.
Now, Steve has access to a medical cannabis prescription through the private provider Curaleaf Clinic, as the NHS is not licensed to prescribe it for Parkinson’s, and his wife Merryl Willis says the change in his wellbeing is “quite remarkable”.
He has been able to go back to his hobbies such as playing walking football, playing chess and card games: all pastimes that were impossible for him to enjoy when his Parkinson’s symptoms were more severe.
“He got his life back,” his wife Merryl, 65, told PA Real Life.

After his diagnosis of Parkinson’s – a neurodegenerative disorder that predominantly affects the dopamine-producing neurons in the brain and can cause tremors, stiffness, and slowed movement and speech among other symptoms – in late 2020, Steve’s world got smaller as his condition deteriorated.
He needed to use an electric wheelchair at home, and the couple – who have been married for six years – made modifications to their home to enable his movement, including removing the internal doors for better accessibility, installing smart home devices so they could communicate throughout the house, and even planning to install a lift so Steve could better get around their home.
Steve had to give up hobbies such as walking football and swimming, could not walk, and experienced tremors which made daily life difficult. Steve’s mind is still fully functional on the inside, Merryl said, but it is hard sometimes for him to process his thoughts and get them out in the world.
“I think about my thinking a lot,” Steve said.
“Parkinson’s, it’s like being surrounded by a firewall, it’s hard to be able to get stuff out. It can come in, but it can’t get out.”

As the years passed, the couple had accepted this new reality, but while on holiday in Jamaica to celebrate Merryl’s 65th birthday in March 2025 they discovered that cannabis had a profound effect on Steve’s quality of life.
Cannabis is decriminalised for personal use in Jamaica, and Steve was offered some by a fellow hotel guest. He had taken cannabis recreationally on occasion in his youth, but was not a regular user and had not used the drug – which is a class B drug under the Misuse of Drugs Act 1971 in the UK – since 1985.
After inhaling vaporised cannabis through the hotel guest’s vape pen, he said the difference was remarkable.
“Eight minutes later… I walked,” Steve said.
“And he didn’t just walk,” Merryl added.
“He stood on one leg and then stood on the other leg… I burst into tears. And the following day, we went down to the beach, and he was jogging through the surf along the beach. And he got his life back.”

Of course, the cannabis Steve took in Jamaica was from a fellow guest rather than prescribed from a licensed provider, so it was unregulated and they did not know the strength nor if it contained any other substances. When they returned to the UK, Steve and Merryl decided to try to get him a prescription for the drug, which has been legal in the UK for prescription by a specialist doctor since November 2018, but soon discovered the NHS is not licensed to prescribe it for Parkinson’s.
According to the NHS, “very few people in England are likely to get an NHS prescription for medical cannabis”. It can only be considered when other treatments are found to be unsuitable or have not helped, and is usually only prescribed for those with rare, severe forms of epilepsy, adults with vomiting or nausea caused by chemotherapy, and people with muscle stiffness and spasms caused by multiple sclerosis.
It is, however, available privately through licensed providers such as Curaleaf Clinic, which Steve contacted to explore his options.
“It wasn’t difficult,” Merryl said of the process of getting a prescription through Curaleaf Clinic.
“You register online, you tell them your problem, you give them access to your NHS history so that they can see what you’ve already tried, because it is important to them that you have exhausted other medical interventions.
“Then you have a meeting with, in Steve’s case, a neurologist consultant, and if they think you’re a suitable candidate, they take it to their multidisciplinary team, discuss it, and if they all agree, (they) issue you a prescription.
“Then you just pay the fee, and your cannabis arrives by courier.”
“I have footage of what happened when Steve first took the properly regulated and licensed and prescribed medication, and it’s quite remarkable,” Merryl continued.
“He walked around the room waving his arms in happiness. He was just overjoyed.
“It’s like he got his life back.”
Since taking the prescribed cannabis, Steve has not needed to use his electric wheelchair at home. He still uses a mobility scooter outdoors, if they are walking more than around two kilometres, but he has been able to go back to playing walking football, which he “honestly never thought he would”.
While Steve’s experience is anecdotal, Parkinson’s UK says there is interest in cannabis-based treatments for people with Parkinson’s because of the way cannabinoids alter how the brain works.
Experiments in labs using animal models or cells grown in a dish have shown potential for cannabinoids influencing both motor and non-motor symptoms of Parkinson’s, but there have been very few clinical trials to test cannabis-based symptoms in people with the condition, so there is not yet enough evidence to give a definitive answer on the drug’s potential positive impact or harms.

Parkinson’s UK research communications manager Becky Jones told PA Real Life: “There is currently a lack of good quality evidence for the safety and benefits of cannabis-based treatments for Parkinson’s. Until we have robust evidence, we can’t formally recommend cannabis-based medicines for Parkinson’s and nor can the NHS prescribe it.
“However, there are new, high-quality clinical trials getting under way to understand if CBD can help manage a range of Parkinson’s symptoms, which is potentially a huge step forward towards much-needed new treatments. We hope to see further trials starting over the next year or two. Anyone considering changing their Parkinson’s treatment or adding new supplements should first discuss it with their healthcare team.”
Licensed prescribers such as Curaleaf Clinic give people the opportunity to test whether the drug may help them, under the supervision of trained medical professionals with a controlled dose that allows users to find the right dosage of the drug’s active ingredients – THC and CBD – that works for them.
Steve’s prescription costs him around £30 per month, and his medical-grade inhaler, which produces vapour rather than smoke and negates the need to mix the medication with addictive, harmful agents such as tobacco, was around a £200 initial cost.
However, Merryl said: “I’d pay 50 times that for Steve to be able to walk again.”

While there are concerns that cannabis contains carcinogens, for Steve that is a risk he is willing to take.
He said: “I’m 72 – in five years’ time I might get cancer, but I’m quite happy to trade cancer in five years’ time for five years of being able to walk.”
Dr Simon Erridge, director of research at Curaleaf Clinic, said: “It is extremely gratifying to see the response that Steve has reported after starting medical cannabis. Unfortunately, there is just not enough research on the traditional motor symptoms that are characteristic of Parkinson’s disease, such as instability, tremor at rest and muscle rigidity. There is somewhat better evidence for non-motor symptoms like anxiety and sleep problems.
“Individual responses can vary considerably, but I hope that through highlighting Steve’s outcomes this is an impetus for further research. We are currently capturing the outcomes from patients, such as Steve, with Parkinson’s disease through the UK Medical Cannabis Registry to examine the real-world outcomes of those with Parkinson’s.
“Ultimately, we need larger, longer studies to truly understand who might benefit and at what doses. For now, medical cannabis should only be initiated for those who haven’t responded or experience intolerable side effects to first line treatments, with realistic expectations about potential benefits and limitations.”
Subscribe or register today to discover more from DonegalLive.ie
Buy the e-paper of the Donegal Democrat, Donegal People's Press, Donegal Post and Inish Times here for instant access to Donegal's premier news titles.
Keep up with the latest news from Donegal with our daily newsletter featuring the most important stories of the day delivered to your inbox every evening at 5pm.