
Bereaved families have said they are “not surprised” that a Sussex-based NHS trust has been rated third worst in the country after “repeated failures” were underlined during their loved ones’ inquests.
The Sussex Partnership NHS Foundation Trust (SPFT), which specialises in mental health and learning disabilities, was ranked 59th of 61 non-acute trusts across the UK in data published by the Department for Health and Social Care this week.
A group of families who believe their loved ones died by suicide “because of failings in care from SPFT” has been formed to highlight the themes they have seen across their cases.
They have identified unprofessional behaviour, oversights in record keeping and a “toxic and harmful” culture in the Trust among the key learnings from their loved ones’ inquests.
Imogen Nunn died in Brighton, East Sussex, on New Year’s Day 2023, having struggled with her mental health since she was 13, her inquest concluded in May this year.
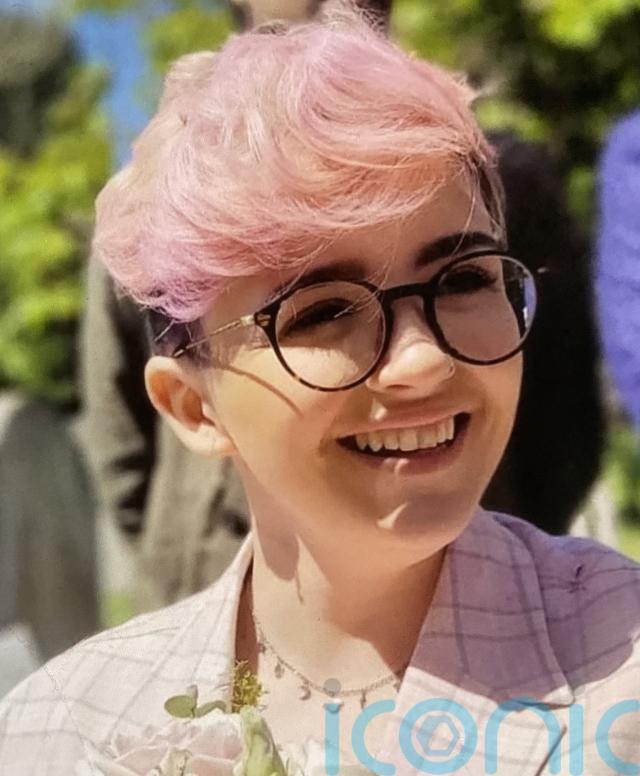
Ms Nunn, who was born deaf, raised awareness of hearing and mental health issues on her social media accounts, which attracted more than 780,000 followers.
Senior coroner Penelope Schofield concluded that “there was a failure by the mental health services to manage her risk” after finding that SPFT practitioners did not review her care plan after a suicide attempt just three months before her death.
The coroner also noted the service “failing to put in place safeguarding measures” after being advised that Ms Nunn had accessed a pro-suicide website and purchased “chemicals to use in suicide”.
Her mother, Louise Nunn, recently joined the bereaved families group and said it’s “not only heartbreaking but alarmingly concerning” to realise other families have been failed by SPFT.
“To me it feels like our loved ones are just another number to them, and there needs to be more serious consequences to all those responsible for failing to fulfil their responsibilities,” she said.
Morgan Betchley, 19, was the mother of a one-year-old boy when she died through a self-inflicted injury on a ward at Meadowfield Hospital in Worthing on March 9 2023.

She was autistic, and had struggled with her mental health for a long time and had been admitted and discharged from mental health units multiple times prior to her death.
Her mother-in-law Louise Hodgson said her death followed six weeks of crisis where Ms Betchley had been “gas-lit, brutalised and traumatised beyond despair” during her care.
At her inquest in November 2024, jurors concluded that evidence showed “repeated failures to follow policies and procedures” by staff at Meadowfield.
They said: “Failures relating to the admission process, understanding of existing diagnosis, risk management, record keeping, family involvement and discharge planning prevented Morgan from receiving access to services she needed at the time.
“We consider it probable that if policies and procedures had been followed, Morgan would have benefited from a level of care more closely aligned to her complex needs,”
They also noted a “failure to act professionally” from some medical staff who refused to accept Ms Betchley’s apology, following an incident where she had kicked out at a nurse during a psychotic episode.
Ms Hodgson, who has worked in the NHS for 33 years, told the PA news agency: “The Trust seems to be led, in terms of its toxic and harmful culture, by psychiatrists with very big voices, and very little notion of what trauma-led care means.
“Leadership and culture are always key, but time and again this trust responds to deaths with tick-box ‘solutions’ and continues to allow staff to exclude and dehumanise desperately ill young people, thus modelling that to junior staff.”
Matty Sheldrick, 29, left A&E and hanged themselves in the grounds of Royal Sussex County Hospital in Brighton having “lost all hope” on November 4, and died on November 22 2022.

Mx Sheldrick, a 29-year-old trans person, who had ADHD and autism, “felt unwanted, othered and rejected” after presenting to hospital in September 2022, his mother has said.
After a 26-day stay, they were eventually discharged as there was no “suitable” bed for them.
During their inquest, Mx Sheldrick’s GP Dr Sam Hall from WellBN told the court there is a “massive gap” in crisis provision relating to mental health.
“There is a gap people are falling into and I feel we’re all just fighting fires trying to keep people safe,” Dr Hall said.
The doctor also highlighted that people who are trans and have neurodivergence are often misunderstood and misinterpreted.
Mx Sheldrick’s mother, Shelagh Sheldrick, said: “A common theme with all families is the lack of care, kindness and compassion shown to our loved ones when in a mental health crisis.”
She added: “I am not surprised and somewhat relieved to hear they have been ranked the bottom of the pile as this has to stop while lives continue to be unnecessarily lost.”
Those rankings are determined by averaging the Trust’s performance against a range of targets, such as reducing waiting times for treatment and for being seen in A&E departments, or improving ambulance response times.
Charlotte Haworth Hird, who represented Ms Betchley’s family during her inquest, noted a “pattern of failures” from the Trust, despite such a number of similar stories.
“It is a sad reality that until SPFT are willing to recognise what is going wrong, to accept responsibility for that, and to make meaningful change, these deaths will continue to happen,” she said.
Dr Oliver Dale, chief medical officer at Sussex Partnership, said: “We are deeply sorry for the loss each of these families has experienced.
“We are absolutely committed to learning and taking action to improve where it is needed. We are working very hard with our staff to make the necessary changes and provide the best quality care to patients that we can.
“The new NHS league tables highlight areas of organisational performance where we need to improve. We are fully focused on doing this on behalf of the patients, carers, families and local communities we serve.”
Subscribe or register today to discover more from DonegalLive.ie
Buy the e-paper of the Donegal Democrat, Donegal People's Press, Donegal Post and Inish Times here for instant access to Donegal's premier news titles.
Keep up with the latest news from Donegal with our daily newsletter featuring the most important stories of the day delivered to your inbox every evening at 5pm.