
A father-of-two with cancer given six months to live after five years of unsuccessful chemotherapy treatments has said he was offered a lifeline with a clinical trial which “cured” him within eight months.
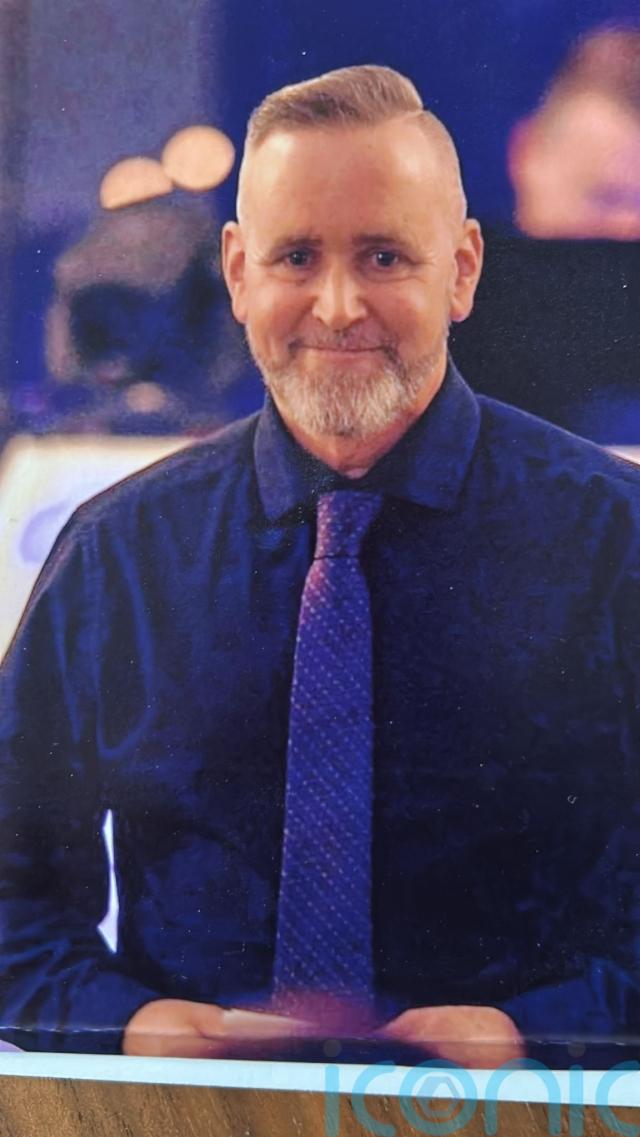
Vaughan Herriott, a former building company owner from Bodmin, Cornwall, was diagnosed with non-Hodgkin lymphoma – a type of cancer which develops in the lymphatic system – in 2017 after going bankrupt and several “family tragedies”.
The 59-year-old said he underwent five different types of chemotherapy over the following five years, but the cancer kept returning – and in 2022, Vaughan was told there were no other treatment options and he only had six months to live.
After fearing “death was a real possibility”, Vaughan said he was offered a lifeline – what he calls his “last chance saloon” – with a place on a clinical trial, which involved giving patients experimental immunotherapy, delivered by infusion.

With this being his “last chance”, Vaughan accepted the offer and started the treatment and, within eight months, he said he was told: “You’re cured, you haven’t got cancer anymore.”
As he prepares to celebrate three years in remission this October, Vaughan is campaigning for further research into cancer treatments alongside the Be Part of Research service, so that others, too, can be offered a “second chance”.
“I basically went from something they couldn’t cure in five years with five different chemos, to being cured in eight months with something that I only had to have once a week,” Vaughan told PA Real Life.
“I would have been dead three years ago if I hadn’t participated in a trial.
“I’m deeply grateful to the fantastic team of nurses and doctors who supported me.”

Vaughan said he had always been “fit as a fiddle” and had once run a successful company in the building trade – but after experiencing financial difficulties, he went bankrupt.
Soon after, he had several “family tragedies”, including losing his father to suicide.
“I remember laughing and joking with him only a week before,” Vaughan said.
During this time, Vaughan had noticed a lump in his neck – but since he had experienced “lumps and bumps” due to problems with his glands since childhood, he said his GP initially dismissed this symptom.

It was not until the lump continued to grow, to the point where Vaughan said it was visibly “sticking out of (his) throat”, that he sought further medical advice.
According to the NHS, the most common symptom of non-Hodgkin lymphoma is a painless swelling in a lymph node, usually in the neck, armpit or groin.
Vaughan said he was advised a biopsy would need to be taken and, in the meantime, he spoke to his GP again.

“Before they biopsied it, I phoned my GP,” Vaughan said.
“They said, ‘We haven’t had any results back or anything, but just out of interest, do you have night sweats?’ And I said, ‘Well, yes, I do have bad night sweats’.
“Then they said, ‘Oh, you’ve probably got cancer then’.”
After doctors ended up removing the entire lump, Vaughan said his stage 3 non-Hodgkin lymphoma diagnosis was later confirmed at the Royal Cornwall Hospital in 2017 and he described it as “shocking”.
He continued: “It was the worst possible news I could’ve received and at a terrible point in my life.
“I went from a dark place to an even darker place.
“I was still grieving for my father, but everything was coming on top of me, all at once.
“There’s nothing like kicking a bloke when he’s down.”

Vaughan, a puppet maker in his spare time and Thunderbirds fan, began a series of treatments, including chemotherapy and Rituximab – a targeted cancer drug.
He said doctors soon increased his dose for the chemotherapy, before moving onto Beam therapy, which destroys cancer cells as well as healthy cells from your bone marrow.
“They harvest your stem cells to give back to you once you’ve had this chemotherapy, which basically kills the bone marrow and any cancer cells,” Vaughan explained.
“You have this chemo, it makes you feel poorly, it kills the bone marrow… and then they give you your stem cells back.
“Since you go neutropenic, which means you have no immune system whatsoever, I was put into isolation for two months.
“After my bloods improved, they allowed me to go home, which was the best day of my life, but the treatment didn’t work.”

Having received five different forms of chemotherapy over five years by this point, Vaughan says, and experiencing side effects of fatigue, nausea and “feeling radioactive”, Vaughan was then told in 2022 the cancer had returned.
He said doctors told him there were no further treatment options for him and he was given just six months to live.
“I was told it had come back again. It had encased my kidneys, it had encased my liver and it had invaded into my spine,” he said.
“After that, they basically said there’s no other chemotherapy that you can have.
“I had to get it straight in my mind that death was a real possibility.”

Soon after, however, Vaughan said he was offered a place on a clinical trial – and by October 2022, after eight months of immunotherapy, which uses uses the immune system to fight cancer, he had reached remission.
“I took to the trial with no side effects and within eight months I was cured,” he said.
Vaughan has now been in remission for nearly three years, and he hopes this immunotherapy treatment will become a “frontline treatment rather than a last chance saloon”.

He said he has always tried to find the positive in every situation and if he could choose one word to sum up his journey, he would say “remarkable”.
He is now supporting the National Institute for Health and Care Research’s (NIHR) Be Part of Research service to help develop new treatments, find better ways to manage health conditions and provide better care.
He has found that mindfulness, spending time with family and “seizing the moment” has helped him process his diagnosis, but his main focus is “encouraging people to step forward and to get more research done”.

“If I wasn’t offered the clinical trial, myself and other people wouldn’t be here,” he said.
“I’ve been given a second chance… and I want to get the message out there that all hope is not lost, even if you feel all hope is lost.
“There’s a light at the end of the tunnel.”
To find out more about the Be Part of Research service, visit: bepartofresearch.nihr.ac.uk/join.
Subscribe or register today to discover more from DonegalLive.ie
Buy the e-paper of the Donegal Democrat, Donegal People's Press, Donegal Post and Inish Times here for instant access to Donegal's premier news titles.
Keep up with the latest news from Donegal with our daily newsletter featuring the most important stories of the day delivered to your inbox every evening at 5pm.